Separating Myth from Evidence
A data‑backed look at what CM really is—and why states, providers, and payers are adopting it at scale.
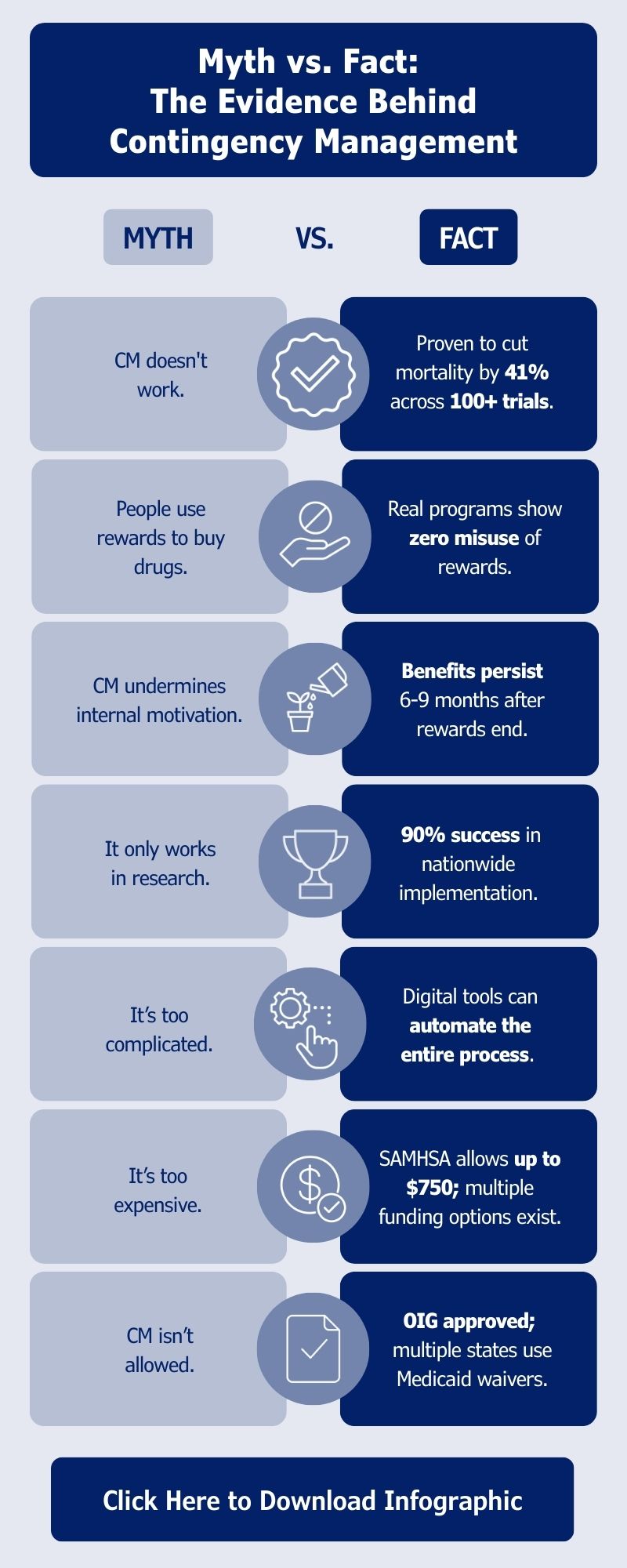
Misconceptions
Even as stimulant‑related overdoses rise, CM remains one of the most misunderstood interventions in the behavioral health field. Questions about cost, legality, and patient motivation often overshadow decades of rigorous research.
This infographic distills the most persistent myths and contrasts them with the actual evidence – including CM’s proven impact on engagement, retention, and mortality. It gives leaders a fast way to understand the science and cut through confusion.
Why it Matters
Contingency management is not new – but the urgency surrounding stimulant use disorder is. Backed by 100+ clinical trials, CM consistently outperforms other behavioral interventions for reducing stimulant use, improving appointment attendance, and increasing treatment retention.
Yet despite federal guidance, Medicaid demonstration projects, and robust data showing zero misuse of incentives in real‑world programs, many organizations still hesitate to adopt CM.
Bottom Line:
Contingency Management is one of the strongest evidence‑based interventions for stimulant use disorder, but outdated perceptions still stand in the way of adoption. As federal agencies expand guidance and more states leverage Medicaid waivers, the opportunity to implement CM has never been clearer.
Digital platforms now make CM simple, compliant, and scalable, allowing organizations to deliver the intervention as intended, and to achieve the outcomes the research promises.