Leveraging Technology-Enabled Addiction Management Changing the Paradigm Substance Abuse Treatment
Patients struggling with substance us disorders (SUD) affects an estimated 320 million people worldwide.1 In 2016 alone, more than 110,000 victims lost their lives to the disease in the U.S. alone.2. Battling the epidemic is challenging for multiple reasons. First, drugs like heroin are cheap and easy to attain, and most home medicine cabinets house some type of prescription painkiller. This ease of accessibility is one reason the disease crosses all sectors of our society; homemakers, teachers, business people — they all now have the same access to drugs as do professional addicts living on the street. While SUD patients may come from different sectors of the population, the addiction’s effect on those individuals generally follows the same progression. Drugs interfere with the rewards center of the brain, along with the judgement center. Addiction makes those struggling lose social consciousness and do whatever they have to do to get the next fix.
Ever-present access to drugs not only makes recovery difficult, it also makes the onramp to addiction that much easier. Psychiatrists like myself, along with law enforcement, are concerned that the expanding legalization of recreational marijuana will only exacerbate the issue of streamlined entrance into substance use, especially for youth populations. Once the barrier to drugs is relaxed, moving on to more dangerous drugs is more likely. When young people succumb to peer pressure to try it “just once,” it can have disastrous effects. Each person’s brain chemistry is unique. While some victims may use for weeks or even months before becoming addicted, others can become addicted after a single use – such as one snort of cocaine or shot of heroin.
Access to treatment is also an issue. Nine in ten SUD patients don’t have insurance, although that number may have risen based on changes in healthcare laws. However, an even more significant issue is that few treatment options are available, especially for those without commercial insurance. If only treatment were as accessible as the drugs.
Co-occurring conditions further the complexities of addiction. Half of all substance use disorder patients also suffer from a mental illness such as anxiety disorder, major depression or bipolar disorder. Treating just the addiction without addressing underlying conditions will not work. Yet that’s the approach traditionally taken by both providers and payers.
One-size-fits-all treatment a no win for addiction
Traditionally, insurers have covered what amounts to cookie-cutter treatment protocols, giving little consideration for each individual’s unique circumstances. A person using a certain type of drug and with a particular mental disorder may need a certain approach for a certain period of time. For another person, it could be totally different. The idea of a one-size-fits-all treatment program is a total myth and has zero scientific support whatsoever. Putting everyone on a conveyor belt program benefits only the provider and payer, not the patient.
The science of recovery
Even with all the complexities of substance use disorders, we now have comprehensive data from scientists, researchers, and brain experts that can be used to predict what types of treatment works best for each patient. We can also use this data to predict when and if a patient is likely to relapse, which is something most patient will experience at some juncture post treatment.
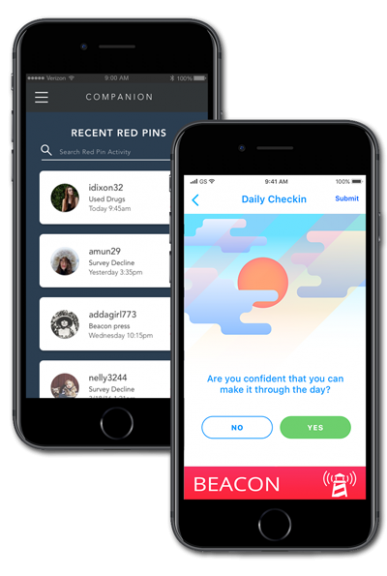
This is why we developed the A-CHESS Platform for relapse prevention and care coordination, including the Connections app for patients, the provider Companion app and robust analytics. Our technology enables payers, providers to identify and monitor key data points in a way that enables proactive communication and, when necessary, intervention.
With the Connections app, patients have 24/7 access to their care team support and peers right in the palm of their hand. It provides continuous access to tools to help them succeed, including a “Beacon” button that patients can push to alert the support team of an impending risky situation or potential relapse. The app also has GPS, which patients agree to enable as part of the program. This intervenes with the patient when they are nearing a potentially risky area, such as where their dealers or friends hang out, and can also alert their counselor or recovery coach.
The Companion app is for the care team (including physicians, counselors, peer coaches, sponsors etc. anymore), who can use it to curate a customized experience for their patients. They can upload and create content and surveys, organize their patients, set up medications and appointments for their patients, message individuals or groups and monitor a patient’s progress.
We have found that when patients have the ability to communicate with their care team in a safe way, it has an ancillary benefit in that it promotes compassion and trust, two essential elements for recovery success. When care team have the ability to be there for patients when and how they need it, the dynamic changes.
Formula for success
Currently thousands of substance use disorder patients have access to A-CHESS and that number is growing through partnerships with behavioral health organizations, rehab facilities, MAT providers, health systems and health plans. Clinical research published in JAMA Psychiatry and the Journal of Dual Diagnosis as well as other publications validate that with A-CHESS:
- 31% fewer patients relapsed
- 50% reduction in severity of relapse
- 71% reduction in readmissions
- 20% more likely to complete treatment
The time to act is now
Substance use is a devastating medical condition, one that destroys lives, tears families apart, and adds billions in costs to an already financially burdened healthcare industry. Reversing this epidemic requires payers and providers work together to create a new approach to treatment, one based on science – not mythology. More importantly, it requires treatment to focus on the entire patient, and to enable continuous, ongoing communication between patients and their care team. This doesn’t happen in healthcare today. Technology is the way to do things differently and create real change quickly.
Substance use victims and their families deserve the highest quality of care and outcomes. Our ability to deliver it is a matter of life or death; there often is no second chance to get it right.
Sources
1 https://www.pbs.org/newshour/nation/u-s-population-reach-320-09-million-start-2015-census-reports
2 http://www.addictionpolicy.org/single-post/2017/12/21/174-a-Day-Understanding-the-Numbers

